Our Chief Medical Officer, Sohail Munshi, is a practicing GP in Manchester and has been for over 20 years. He is responsible for leading the clinical strategy of MLCO and TLCO, aiming to improve population health and wellbeing by turning the strategy into reality. Sohail’s latest blog is about Population Health Management, what it means and why it is important.

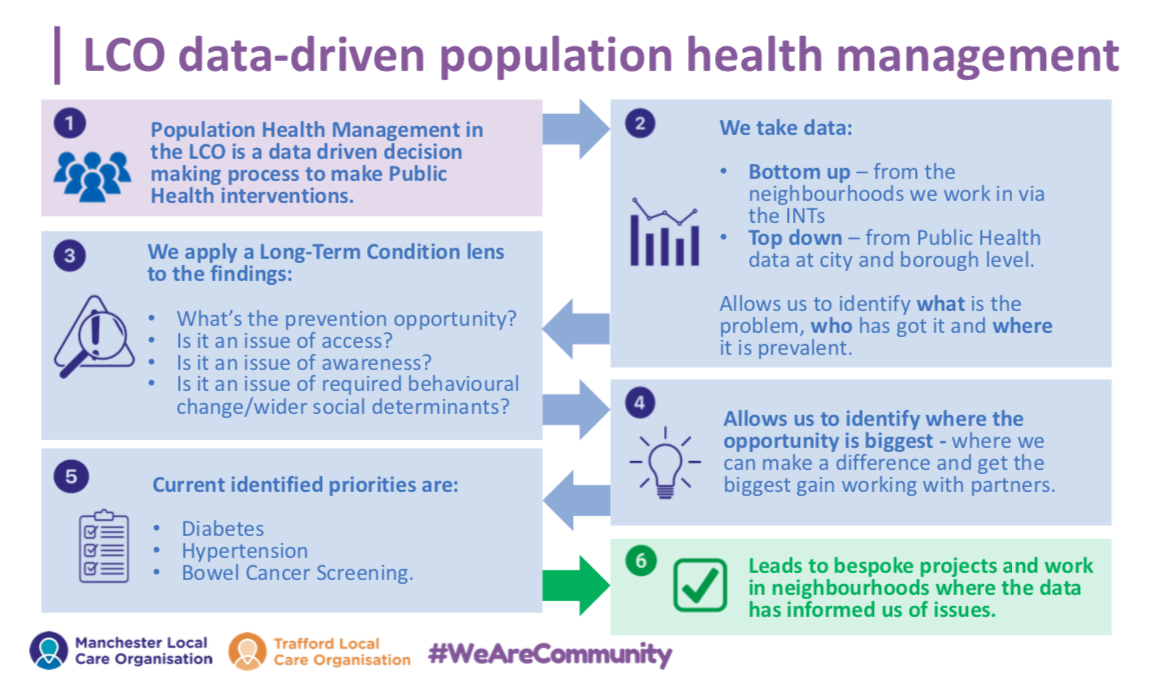
Population Health Management (PHM) is a term you might have heard but might not fully understand. It’s one of the key strategic priorities for us in the Local Care Organisations, and it’s something everyone can play a role in.
In simple terms, PHM is largely about improving health through prevention and early identification of the things that impact on a lot of people’s health. Obviously, there are multiple conditions and risk factors that impact on people in our communities and it’s impossible to tackle everything at once.
That’s why our PHM approach is about using data to inform us. We take data bottom up – from the neighbourhoods we work in – and top down – from Public Health data at city and borough level. It allows us to identify what’s the problem, who has got it and where it is prevalent. We can then identify where we can make the biggest difference working in the community. In particular it helps us work with under-served communities and reduce health inequalities in a more proactive way.
This year (2023-2024) we’ve identified three key PHM priorities – Bowel Cancer screening, Hypertension (high blood pressure) case finding and Diabetes. Using the LCO neighbourhood approach we’ve been able to target work in the communities where we can make the biggest difference and we’ve seen some fantastic progress.
We’ve worked with primary care and other partners on ‘eat well, get well’ diabetes educational programmes, we have a fantastic community-led blood pressure check programme delivered by the LCO and Nuffield training community volunteers in Ancoats, Clayton and Bradford; and there’s lots of targeted work across the neighbourhoods on encouraging people to use their bowel cancer screening kits. All of these examples are about working with GPs, local people and the voluntary sector to support the people and communities most at risk.
The work is so important because it will make a real difference to health outcomes. Looking at Bowel Cancer screening, we know that screening reduces chances of advanced bowel cancer by 34% and death by 40%. Our screening rates are only 56% in Manchester (compared to 69% in the UK) but the work we’re doing is seeing this figure rise. That means earlier identification of possible cancers, less invasive treatment for people and better outcomes. In Hypertension we know that even a small rise in high blood pressure increases the risk of heart disease and stoke by up to 10% per year, year on year. Our work has contributed to a further 4,000 people being identified as having high blood pressure so far this year. They can now be supported with the right advice and action to prevent more serious issues in the future.
When you consider these stats, you can quickly start to visualise the long-term benefit that this work will have. That’s not only in reducing the risk for the individual, but also reducing the future pressure on hospital, community and social services if just a proportion of those people can avoid the consequences.
That’s why PHM is such an important priority for the LCO and why we focus on it. The work of our teams and our partners in primary care, public health and the wider community in this field is potentially game-changing.
Think about your role in this as well as a member of staff or a member of the community. Think of the impact you can have if in each contact you have with people, where it’s relevant, that you ask if they’ve completed their Bowel Screening kit, if they know their blood pressure, if they’re aware of diabetes education. By making every contact count in this way we can all play a part in improving the health of the population in Manchester and Trafford.
Follow Sohail on Twitter/X